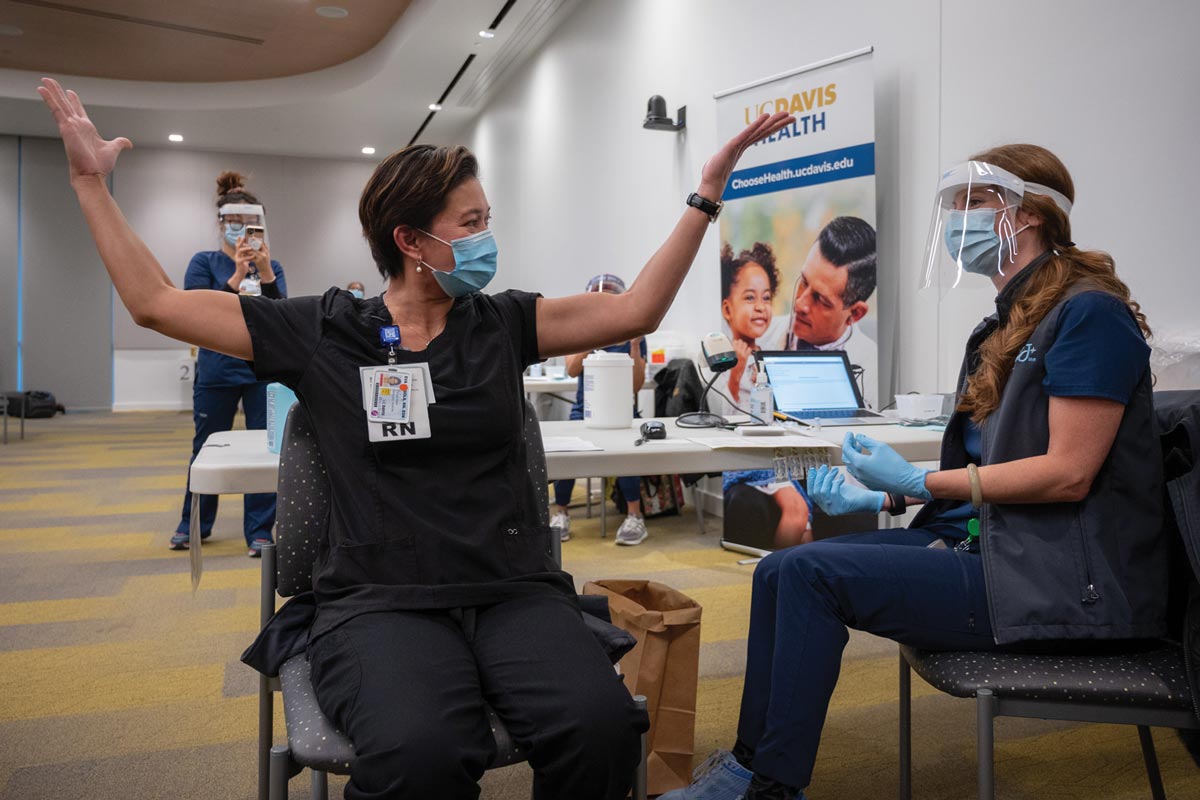
LAST month, Eva Teniola kicked off Sacramento, California’s vaccination campaign as she became the city’s first health care worker to receive a dose of the Pfizer-BioNTech vaccine.
Three weeks later, Teniola, a 47-year-old emergency room nurse at UC Davis Medical Center, received her second jab on January 5 and completed the process to be fully inoculated.
The Pfizer-BioNTech vaccine is 95% effective against COVID-19, and must be administered in two doses 21 days apart, according to the Food and Drug Administration.
The path to hope and protection after a grim year outweighed the “tolerable soreness” the nurse felt on her left arm into the next day.
“I feel thankful, proud, honored, and hopeful for the safety of myself, my patients and my loved ones,” Teniola told the Asian Journal.
Her experience mirrors that of hundreds of other health care workers across the country who have been on the frontlines of the devastating virus since last March.
And while both the Pfizer-BioNTech and Moderna vaccines’ record development and arrival in the U.S. offered some reprieve, the daily infection and fatality numbers remind of the sobering reality and the infectious nature of the virus.
In Teniola’s case, she continues to witness numerous deaths working in the emergency room, especially in individuals over the age of 45.
“These ages supposedly are the prime years and best time to travel or spend quality time with family and friends, but instead, because of the deadly COVID, we have to isolate ourselves from our loved ones,” she said.
For Emmanuel Bando, a nurse manager of ambulatory care at Lincoln Medical and Mental Health Center in New York, his turn to get vaccinated came as a blessing because he initially wasn’t prioritized since he does not work in an emergency room or intensive care unit. But, he made his case for being vaccinated as overflow COVID patients have been sent to his unit.
During the first round of the Pfizer-BioNTech vaccine, he reported muscle weakness and a spike in blood pressure, but did not experience other side effects other than soreness at the injection site the second time.
He completed his vaccine on January 12, which made him “feel more confident and effective” in stopping the spread of the virus.
“Right now, in our hospital, we have 60 cases and I found out that the other Health and Hospital [locations] are sending their COVID patient to us,” Bando told the Asian Journal. “The really sad part is that they removed my three ambulatory care nurses to work in the inpatient units and left me with [a] skeletal crew.”
As of this writing, the United States passed the 24 million mark of total cases and over 400,000 deaths.
In California, three areas — the Bay Area, San Joaquin Valley and Southern California — continue to be under the state’s regional stay-at-home order as their ICU capacities are well below the 15% threshold. The state confirmed over 2.97 million cases to date with a seven-day positivity rate of 10.6%.
Los Angeles County over the weekend became the first county in the country to hit 1 million cases, and estimates show that 1 in 3 residents have been infected at some point, according to the Los Angeles Times.
“The public needs to be reminded that the vaccination does not provide full protection from COVID-19 right away as it takes some time for the body to develop immunity to it,” Anna Medrano, a nurse practitioner at City of Hope in Duarte, California, told the Asian Journal. “Collectively, we can help control the staggering number of new cases by continuing to practice social distancing, wearing a mask and practicing other infection control measures. Continue to stay informed and stay healthy for the sake of our loved ones, our communities and our country.”
Medrano, who was the first at her hospital to receive the Pfizer-BioNTech vaccine last month, got her second dose on January 4.
Similar to the first round, she experienced a slight fever, generalized body aches fatigue, and tenderness on her left arm afterward. She seeks to dispel any misinformation about the side effects of the vaccine.
“For those planning to receive the vaccine, please plan ahead of time. If you can, take Tylenol or ibuprofen before getting your vaccination and plan to take the vaccine when you can stay home and take care of yourself for one to two days, depending on your symptoms,” she said. (Editor’s note: Check with your physician before taking any medication like ibuprofen or acetaminophen before and after your vaccination.)

Setting an example
For every individual who gets vaccinated, there is the other side of those who are still skeptical, despite studies showing the safety and efficacy of the Pfizer-BioNTech and Moderna vaccines.
Still, health care workers are pleading with colleagues and those eligible in the next tier to complete their injections and trust the science.
“Let’s be encouraged. If not for yourself, think of your loved ones and the future of humanity. COVID is like the lottery: if you get it, you may have mild side effects, or you get it big time, that you get sick and die. We don’t know what effect COVID will bring until you get it. So, get vaccinated before COVID gets you,” Teniola said.
Jesse Caloza, an operating room orderly, said getting the vaccine was the “most important decision” he’s made in his 25 years working at an Orange County-area hospital.
“Taking the COVID-19 vaccine was the most important decision I’ve had to make in my 25-year career at the hospital. It was also one of the easiest. I hope all health care workers, especially my kababayans, take it,” Caloza told the Asian Journal. “The fight against COVID-19 isn’t over, but taking the vaccine means we are one step closer. We must do everything we can to protect ourselves, our patients, our families, and our community.”
For Dr. Antonio Moya, a neurologist and public health advocate, getting both rounds of the vaccine goes further than protecting himself and his patients — but to provide an example for the greater Fil-Am community as LA County is set to roll out vaccinations for individuals 65 years and older.
“I recommend all Filipinos to be proactive and ask their primary care providers about when they can be considered for the vaccine. It would be great for younger Filipinos to also help advocate for their elderly parents or grandparents to get the vaccine as soon as possible,” Moya, who completed his second dose on January 8 as part of LA County’s effort to vaccinate health care workers, told the Asian Journal.
However, Moya cautioned that being inoculated is not “a free ticket” to engage in nonessential travel and to forget the public health precautions that have become part of the new normal.
“Regardless of vaccination or not, our community needs to stop the spread through public health…These actions are the easiest ways to prevent overwhelming our hospitals nationwide,” he said.
Dr. Joyce Javier, a pediatrician and researcher at Children’s Hospital Los Angeles, echoed the importance of the community to be protected, given the numerous factors that have contributed to Fil-Ams being at higher risk — being employed in frontline, essential services like the medical field as well as living in multigenerational households.
“It’s important for our health care workers to model to our community that the vaccine is safe and that can help alleviate fears about the vaccine,” Javier told the Asian Journal, citing National Nurses United’s findings that Filipino nurses make up 31% of COVID deaths, despite only being close to 4% of the nursing population in the U.S.
She added, “I hope my story can encourage others to get the vaccine when it’s available to them. My hope is that having the vaccines available will help address not only the health impacts of the pandemic, but also the mental health impacts of COVID-19 on all our communities.”
Javier and Moya shared culturally relevant resources, including the Filipino Family Health Initiative, a program that is offering parenting workshops; and Tayo Help, an online platform with expert-backed articles to dispel any COVID misinformation, as Fil-Ams continue to navigate the pandemic and wait for the opportunity to get vaccinated.
“There’s obviously a lot of anxiety among all communities and also with our teens, children and health care workers. I think it’s just important to keep the communication lines open in the family,” Javier said.