By Samantha Young/Kaiser Health News
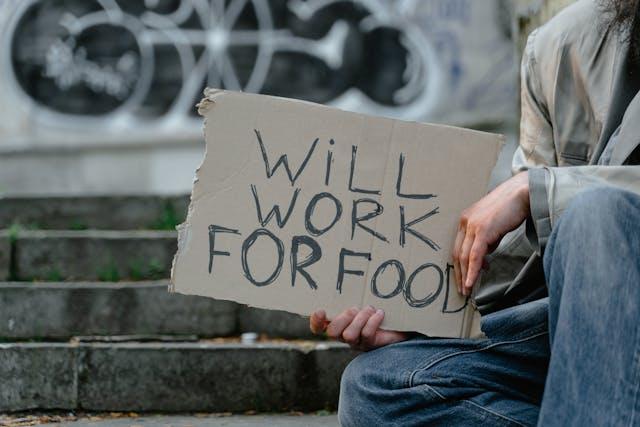
SACRAMENTO — When Johanna Trenerry found a nursing home for her husband after his stroke, she expected his stay would be temporary.
He never came home.
Arthur Trenerry died at Windsor Redding Care Center in Northern California in October 2020. The 82-year-old great-grandfather is among more than 9,900 California nursing home residents who have died of covid-19.
The nursing home where Trenerry died is licensed by the state, but not under its current owner, Shlomo Rechnitz. The state denied Rechnitz a license, citing at least one death and multiple cases of “serious harm” at other nursing homes he owns or operates. To get around that, Rechnitz formed a business partnership with one of the home’s former owners, who continues to hold the facility’s license.
Some California lawmakers want to put an end to those types of business arrangements and ban people or entities from buying or operating nursing homes unless they have a license — which is the situation in most states. They’re also proposing an overhaul of the licensing process to reject applicants with poor performance and those without adequate experience or financial resources.
The ambitious effort, which the industry considers an overreach, could make California’s oversight the gold standard and a model for other states trying to improve nursing home care. Nationwide, more than 152,000 residents of nursing homes have died of covid during the pandemic, according to federal data.
“The public health emergency that we’ve experienced could be something that becomes a catalyst for making real change,” said Dr. Debra Saliba, a UCLA professor of medicine who served on a National Academies of Sciences, Engineering, and Medicine committee that released a comprehensive report on nursing homes in April. “One of the things that we have right now is the determination, the resources to make things happen.”
In his State of the Union address in March, President Joe Biden said the quality of care had declined in nursing homes taken over by investors — and vowed to set higher federal standards. In anticipation of the speech, the White House released a proposal calling on Congress to boost funding for nursing home inspections and to give federal regulators the authority to deny Medicare funds to underperforming facilities. The administration also directed the Centers for Medicare & Medicaid Services to propose minimum staffing standards within a year.
States are also taking steps to improve quality. New Jersey, for example, this year adopted a law that toughens penalties for health violations and requires nursing homes to disclose financial records.
In California, lawmakers are considering several proposals, including the changes to nursing home licensing rules.
Companies and individuals can buy or run nursing homes in California before they get a license, a process that even an industry lobbyist described at a legislative hearing this year as “backward” and unique to the state.
“In California, nursing home owners and operators can operate without a license even after they’ve been denied a license,” said state Assembly member Al Muratsuchi (D-Torrance), author of AB 1502. “Many of these owners and operators have, unfortunately, an extensive history of neglect and abuse.”
Muratsuchi’s bill would require an owner or company to apply for a license 120 days before buying or operating a nursing home and include financial records that contain the names of all owners and investors. The state would reject applicants who fail to meet standards for character, performance in other homes, and the financial ability to run the home. Homes operating without a license would lose Medicaid funding and couldn’t admit new residents.
The powerful California Association of Health Facilities, which represents more than 800 nursing homes, has blocked previous licensing legislation and has set its sights on Muratsuchi’s bill. The group is led by Craig Cornett, a veteran of the state Capitol who has worked for four Assembly speakers and two Senate leaders.
The organization has made just over $2 million in political contributions and spent $5.9 million lobbying lawmakers from Jan. 1, 2011, through March 31, 2022, according to records filed with the California secretary of state’s office.
The bill fails to consider the state’s “complex regulatory environments” and would create “extensive” disclosure requirements on ownership applications that “in many cases would fill an entire room with boxes and boxes of paper,” Jennifer Snyder, a lobbyist for the association, told lawmakers in January.
The measure would “eliminate the ability for most current owners in California to actually apply or even apply for a change of ownership,” she added.
But this year, the industry faces an altered political landscape.
Covid has pushed lawmakers to act — and Muratsuchi has gained a valuable co-sponsor for his bill, Democratic state Assembly member Jim Wood, head of the Assembly Health Committee. Wood has condemned nursing homes for not doing enough during the pandemic and has directed state regulators to conduct stricter oversight.
Muratsuchi’s measure has cleared the state Assembly and awaits a hearing in the Senate.
Investigations by news organizations CalMatters and LAist last year found that at least two California nursing home operators without licenses were running dozens of facilities even though officials at the state Department of Public Health had declared them unfit to do so.
The homes remain open, in large part because finding another nursing home for residents is incredibly difficult.
In July 2016, state regulators denied a license to Rechnitz — who had purchased the Windsor Redding Care Center, where Arthur Trenerry died — citing 265 health and safety code violations at his other facilities in the previous three years. Nevertheless, Rechnitz continues to operate the home in partnership with a former owner, Lee Samson, who is listed as a license holder in state records.
Mark Johnson, a lawyer who represents Rechnitz and his company, Brius Healthcare, said that Windsor Redding Care Center’s “license is in good standing” and that Rechnitz is managing the facility under an agreement “that is customary in the skilled nursing facility industry.” Rechnitz has filed a new and updated license application with the state, Johnson said.
Johanna Trenerry said she had no idea Rechnitz had been denied a license. Had she known, she said, she would never have placed her husband of 60 years at Windsor Redding.
Even before her husband caught covid, Trenerry and her children were trying to transfer him to another home because he seemed overly medicated, could no longer hold up his head, and fell numerous times trying to get out of bed, she said. Once, she recalled, the nursing home brought out the wrong person when the family visited.
They kept him “so drugged up,” said Nancy Hearden, one of the Trenerrys’ eight children. “And I think it was just because it was easier for them. He wasn’t getting to go to his rehab. I felt, ‘We’ve got to get him out of this place.’”
Then he got covid.
Sixty of the 84 residents at the facility came down with the disease in September 2020 — and at least two dozen of them died. According to a lawsuit filed by family members of 15 residents who died, including the Trenerrys, employees of the home were forced to work despite having covid symptoms. The lawsuit refers to state citations that found the home didn’t supply enough personal protective equipment to staffers, didn’t test staff, and placed covid patients and untested patients in the same rooms with residents who weren’t infected.
Johnson denied the allegations.
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.