SACRAMENTO — With the rapid spread of the COVID-19 omicron variant across the state, Covered California is urging uninsured and eligible individuals to act now so that they can have comprehensive health care coverage for all of 2022. Coverage is critical to both getting needed preventive care and covering the costs of unforeseen care. The first enrollment deadline is fast approaching, and Californians need to sign up before the end of the year in order to have their health care coverage be effective on Jan. 1.
“Covered California is urging everyone who needs coverage to check out their options and sign up, before the end of the month, so they can start the New Year with protection and peace of mind,” said Peter V. Lee, executive director of Covered California. “The COVID-19 pandemic continues to highlight the fact that life can indeed change in an instant. With the omicron variant surging across the state, every Californian should be sure to have coverage and take the needed steps to stay healthy and safe.”
Californians who sign up by Dec. 31, and pay their first bill, will have their coverage take effect on Jan. 1.
COVID-19 hospitalizations in California average $127,000 for complex care
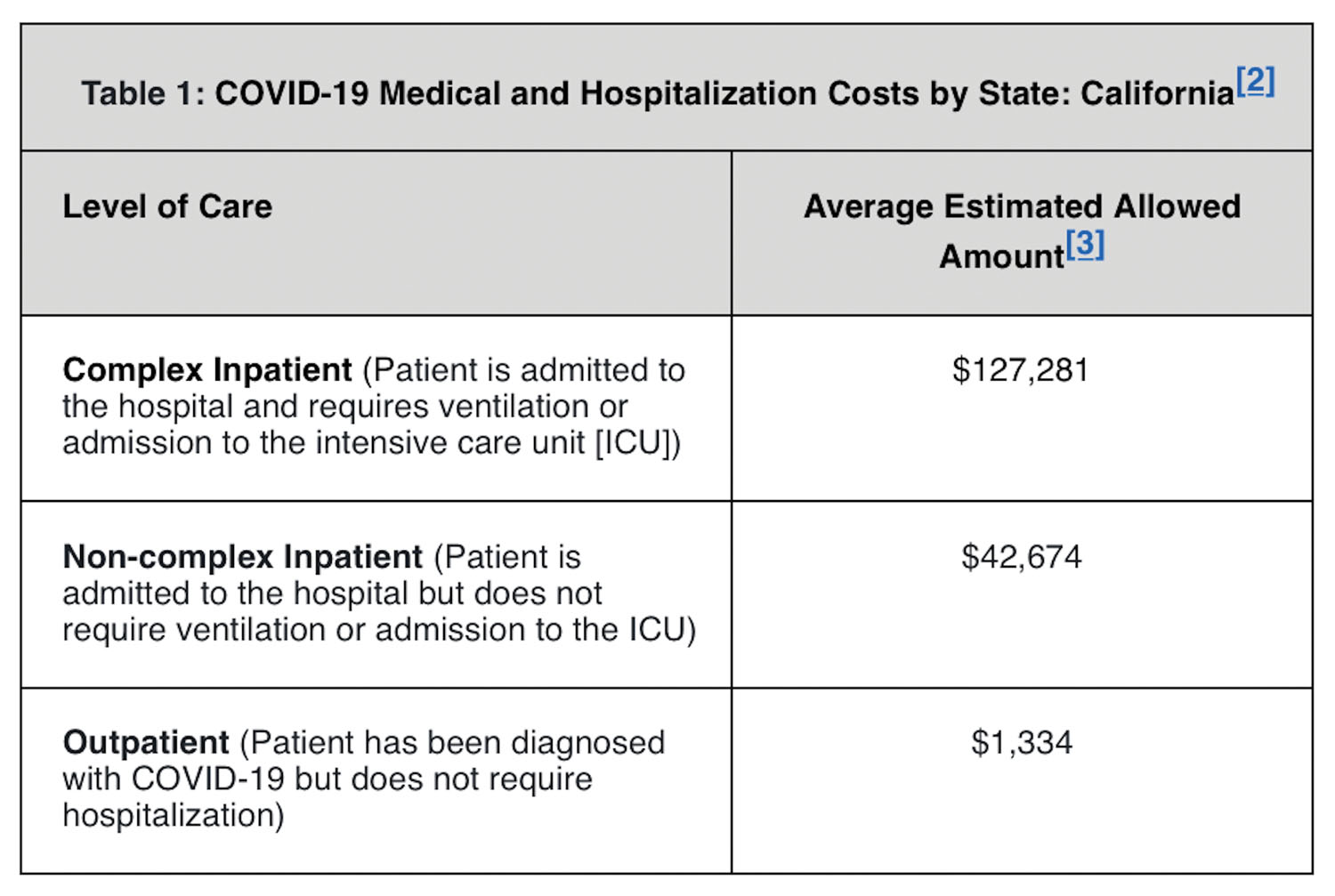 A national nonprofit group recently analyzed claims data across the country and examined cases of COVID-19 in which patients were admitted to the hospital and required ventilation or admission to the intensive care unit (ICU), which is much more likely to occur among the unvaccinated. FAIR Health, which manages the nation’s largest database of privately billed health insurance claims, found that the average cost for a complex care COVID-19 hospitalization was $127,281 in California.
A national nonprofit group recently analyzed claims data across the country and examined cases of COVID-19 in which patients were admitted to the hospital and required ventilation or admission to the intensive care unit (ICU), which is much more likely to occur among the unvaccinated. FAIR Health, which manages the nation’s largest database of privately billed health insurance claims, found that the average cost for a complex care COVID-19 hospitalization was $127,281 in California.
In cases where a patient needed to be hospitalized, but did not require ventilation or admission to the ICU, the average cost in California was $42,674, which is virtually identical to the average costs for Covered California enrollees who are admitted to hospitals for all reasons.[1]
Finally, for patients who were diagnosed with COVID-19 and received only outpatient care — which is much more likely for people who have been vaccinated and received their booster shot — the average cost in California was $1,334. For those with insurance, only a small fraction is paid out-of-pocket by the consumer.
“No one wants to end up in an emergency room or hospital for COVID-19 or any other reason, but if you do, a quality health insurance plan through Covered California can save you tens of thousands of dollars,” Lee said. “In addition, having health insurance means you are more likely to get preventive care and regular treatment for chronic conditions, which helps keep you out of the hospital in the first place.”
Significant savings for more than 1 million uninsured Californians
Signing up for quality coverage is more affordable — for more people — than ever before thanks to the increased subsidies provided under the federal American Rescue Plan that took effect earlier this year.
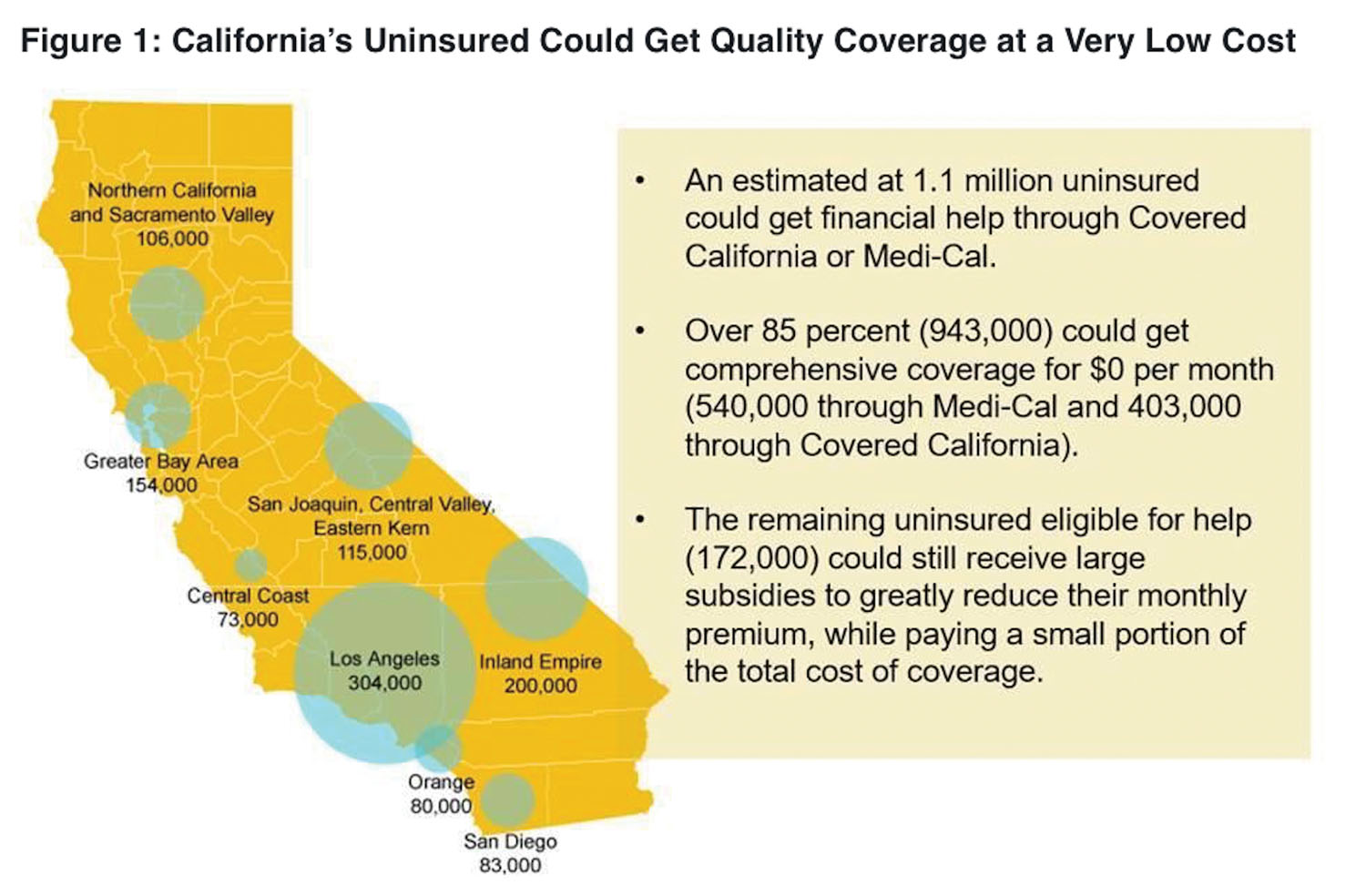
An estimated 1.1 million Californians are uninsured and eligible for financial help. The vast majority of the uninsured, more than 940,000 people, are able to get coverage through either Covered California or Medi-Cal at no cost.
Californians who do not qualify for a $0 premium will still likely see significant savings through the increased financial help available due to the American Rescue Plan. Right now, more than half of Covered California enrollees are paying less than $10 per month, and 75 percent are paying less than $100 for their brand-name health plan.
“Many of the people who are uninsured right now do not know they are eligible for financial assistance, or they have not checked recently to see how affordable quality coverage can be,” Lee said. “Do not wait until the last minute, or let the Dec. 31 deadline pass, without checking your options.”
In addition, the American Rescue Plan provides financial help to many middle-income families. These middle-income families who earn more than $106,000 a year, and were previously ineligible for federal assistance, are now saving an average of nearly $800 a month on their health insurance premiums.
The financial help for middle-income consumers can also benefit those who are currently insured directly through a health insurance company. An estimated 260,000 Californians have direct coverage and can switch to Covered California, and potentially get the same health plan, and save hundreds of dollars per month.
“Visit CoveredCA.com, where you can see the health plans available in your area and how much you can save on the coverage you’re already paying for,” Lee said.
Consumers can easily check out their eligibility and options at CoveredCA.com
Those interested in applying for coverage can explore their options — and find out whether they are eligible for financial help — in just a few minutes by using the Shop and Compare Tool at CoveredCA.com. All they need to do is enter their ZIP code, household income and the ages of those who need coverage to find out which plans are available in their area.
In addition to signing up consumers through its website, Covered California also partners with certified and licensed enrollers who provide free and confidential help throughout the state. Covered California works with more than 11,000 Licensed Insurance Agents, who have established more than 500 storefronts in communities across California.
These storefronts feature Covered California signs and logos and provide consumers with a local point of contact to answer questions and help them enroll in a health plan that best fits their needs, whether through Covered California or Medi-Cal, depending on their eligibility. Consumers can visit https: //www.coveredca.com/support/contact-us/ and search for the agent nearest them.
Consumers can also call Covered California at (800) 300-1506 and get information or enroll by phone.
Signing up for a health plan will also help Californians avoid being subjected to the state individual mandate. Consumers who can afford health care coverage but choose to go without could pay a penalty when they file their state taxes in 2023. The penalty is administered by California’s Franchise Tax Board, and could be as much as $2,400 for a family of four.
Open enrollment runs through Jan. 31
Covered California’s open-enrollment period runs through Jan. 31, 2022 — unlike the federal deadline, which is Jan. 15 for states that use healthcare.gov. Consumers who sign up after Dec. 31 will have their coverage start on Feb. 1.
Covered California’s online enrollment portal and certified enrollers will also help people find out whether they are eligible for Medi-Cal. Medi-Cal enrollment is available year-round, and the coverage will begin the day after a person signs up. In addition, people can apply for Medi-Cal online or by picking up an application at one of the many county resource centers throughout the region.
Covered California is the state’s health insurance marketplace, where Californians can find affordable, high-quality insurance from top insurance companies. Covered California is the only place where individuals who qualify can get financial assistance on a sliding scale to reduce premium costs. Consumers can then compare health insurance plans and choose the plan that works best for their health needs and budget. Depending on their income, some consumers may qualify for the low-cost or no-cost Medi-Cal program.
Covered California is an independent part of the state government whose job is to make the health insurance marketplace work for California’s consumers. It is overseen by a five-member board appointed by the governor and the Legislature. For more information about Covered California, please visit www.CoveredCA.com.